Hi all, Cassie here, and it’s been awhile since I’ve neeped out on a particular teaching topic. This one is near and dear to my heart (*ba-dum-ching!*) so here we go, with the usual caveats — I am neither your cardiologist, nor am I a cardiologist, this is just an armchair overview for people who’ve wondered what the hell EKGs show and how the heck they work.
(Someone has told me this is especially timely now, given how many personal heart trackers, etc, there are out there on the market, so hooray! Happy to be of service.)
If you’ve ever watched an ER-style show, you’ve seen an EKG. In fiction and reality they come in two flavors — the top green line on the hospital monitor, that’s watching your heart rhythm live-time — it’s the one that can make the dramatic beeps and boops if you set your monitor for sounds, so you can get that good ‘oh no, we’re losing him!’ flatline action in:
And you might’ve seen a more in-depth 12 lead EKG print out that looks like this:
What’s occurring in both cases is we’re acquiring a 2D graphical representation of the 3D beating of your heart muscle, inside your body.
This is accomplished by us putting assorted leads on you, depending on how thorough a view we want to get, so that the machine can essentially check the resistance your body has as small currents go through it, directionally, from one lead to the next.
We’re looking for injured muscle tissue, as injured muscle tissue conducts differently — and if you’re having a heart attack, we may be able to save you/heart-tissue-cell-function if we act quickly enough. And we’re also looking for conduction abnormalities, wherein the nerves controlling your heart aren’t acting in synch, and maybe you need a pacemaker or some medications to straighten them out some.
(Don’t worry, we’ll get way into more depth here in a sec. I’m just dropping in slow.)
Sometimes the leads provide the on-going green-line, which is called ‘telemetry’ in the hospital — ie someone on a tele-floor, or in a tele-bed, has leads on them that are monitored at all times (these are a given in the ICU, as well), because we’re worried something might happen with their heart in a way that we’re not worried about a patient in a typical med-surg bed.
But if someone who’s unmonitored in a med-surg bed starts acting up, pulling a Fred Sanford on us, telling us that their heart hurts and they don’t feel right — we’re gonna slap enough leads on them for that 12 lead like you saw above, so we can get a good window into their heart’s functionality and see if it’s behaving right.
How can we tell what’s going on from just looking at the lines on an EKG?
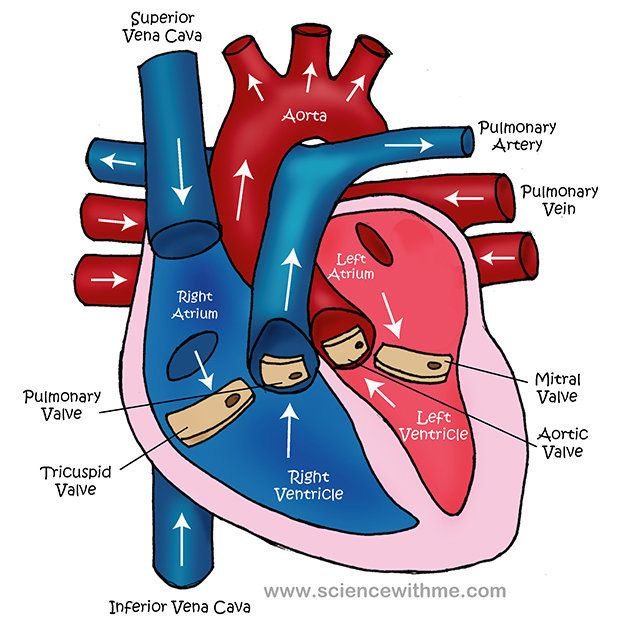
Let’s talk a little bit about heart anatomy.
As a muscle, your heart is responsible for your entire circulatory system, pumping oxygenated blood out via arteries to your entire body (every cell you have! all 37 trillion of them!) and then much more passively receiving that deoxygenated blood (after your cells use that O2) back in via venous return, then sending it into your lungs to be re-oxygenated, so the whole cycle can begin again.
To do this, your heart is comprised of four chambers, the atria up top, and the ventricles down below. The atria are kinda like the staging ground for blood movement, whereas the ventricles are the part that does all the heavy pushing.
Just like a car engine needs all the parts to be working in a coordinated fashion to keep your car moving forward, so does your heart in regards to blood and your bodily functions. And if anything gets out of whack, an EKG can let us see where and perhaps why.
What controls your heart? Nerves — here’s a pic!
Your SA node (aka sino atrial node, aka your heart’s pacemaker) manages your atria, and sends a message to the AV node to pump the ventricles.
So already we’ve got a time-delay there, right? Your whole heart isn’t pumping instantaneously, all the time — otherwise you wouldn’t have a separate lub to your dub.
The atria fill, they squeeze that blood down into the ventricle, and then the ventricles squeeze it out to either your body or the lungs.
It is always (supposed to be) a two step process.
Now let’s take it to the EKG!
Graphically, normal sinus rhythm is what we’re aiming for, as show below:
(I’m not gonna get 100% numberswise with you, but just know that each of the pink grids on a 12 lead EKG represent discrete increments of time.)
In normal sinus rhythm, each piece of the heart squeezes at the correct time, in the correct order, to successfully pump blood around your body. This is the optimal rhythm/timeframe in which this flow occurs.
Now let’s break it down piece by piece!
The P wave there?
That’s indicative of your atrial action — the muscles in your atria polarizing and depolarizing as the electrical charge from the SA node goes through them.
Occasionally you’ll see P-wave abnormalities inside the P-wave itself:
And those are indicative usually of mechanical issues with the muscle/valves of the heart.
But you can also see atrial fibrillation (aka A-fib) and atrial flutter.
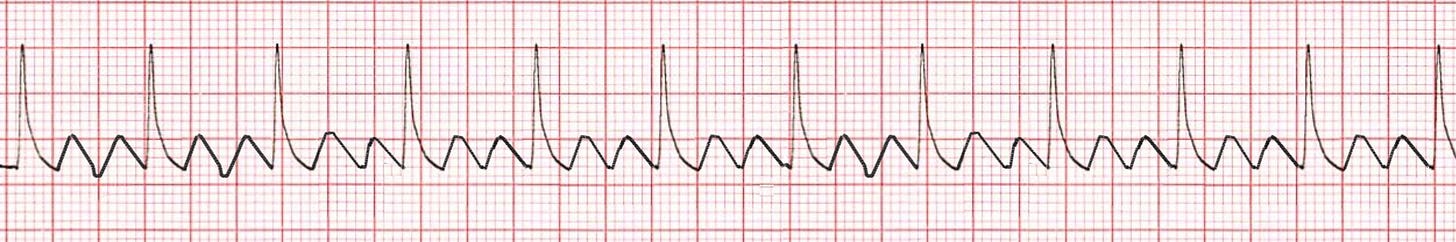
Atrial flutter looks like this, and you don’t have to be a nurse to know that something’s wrong with it, if you compare it to the normal sinus rhythm up above:
Look at all those p-waves! They’re sawtoothing all over the place! (This is the technical term and not just me making up metaphors! ;))
And atrial fibrillation also looks worrisome:
Man, that atria can not figure out what it is doing! It doesn’t know when to fire!
The problem with both of these rhythms is that they’re not promoting optimal blood flow.
Your atria and ventricles have a pact, right? They’re eternally handing off this baton of blood, back and forth, back and forth.
But if your atria try to hand your ventricles blood at the wrong time, or can’t figure out how much blood — or are unable to squeeze as much blood, because they’re simply going too fast to function — then your body’s going to (possibly) have problems.
One of the main consequences of living in a-fib or a-flutter — because sometimes these conditions are intermittent, and/or not always immediately life threatening — and not knowing it, is that inadequate emptying allows for a portion of the blood in the atria to be left behind. And if that blood hangs out with other blood too much, it’s possible to get a clot. And if that clot makes its way into the ventricle — your ventricle doesn’t know any better! It’s gonna keep pumping —
Which means that clot might shoot up right into your brain and cause a stroke. (Another topic, soon, I promise!)
This is why a lot of elderly people (women in particular) are on blood thinners — because they can’t fix the conduction issue (for whatever reason) and so the only way to protect them from clots/strokes is to stop their blood from clotting as well.
(Sadly, this them puts them at risk for head bleeds after falls — but stay tuned for future posts about strokes, k?)
Okay, I’ve avoided my book for long enough for today, let me get back to fiction writing — don’t worry though, we’ll hit the QRS segment and your ventricle function on Monday!
— Cassie










I get the quick five-minute heart check about every 6 months. But about 5 or so years ago, I had a 30-minute (45?) check that involved lying on my side, and someone pressing something on me - that revealed that I supposedly have a "mild interior mitrial regurgitation" or something.
Not sure which is the EKG, and which is called something else. Think I'm due for the long one again soon.